Diagnostic Laparoscopy
What is a Diagnostic Laparoscopy
A diagnostic laparoscopy is the use of a fibro optic laparoscope to visualize the structures and organs within the abdominal cavity, and pelvic cavity. A diagnostic laparoscopy is a minor operation.
When will I need a Diagnostic Laparoscopy?
Its purpose is to investigate causes of abdominal pain of unknown origin. There are many causes of abdominal pain including inflammation of an organ, adhesions, infection, internal bleeding, fluid accumulation, undiagnosed abdominal mass or and unexplained liver defect. A diagnostic laparoscopy may also be used to obtain a peritoneal washing. Your surgeon will use a saltwater solution to wash the peritoneal cavity. Once the solution, along with cells from the peritoneal cavity, is retrieved, it’s sent to a laboratory to be analyzed for cancer cells in a test called peritoneal cytology.
What happens during the operation?
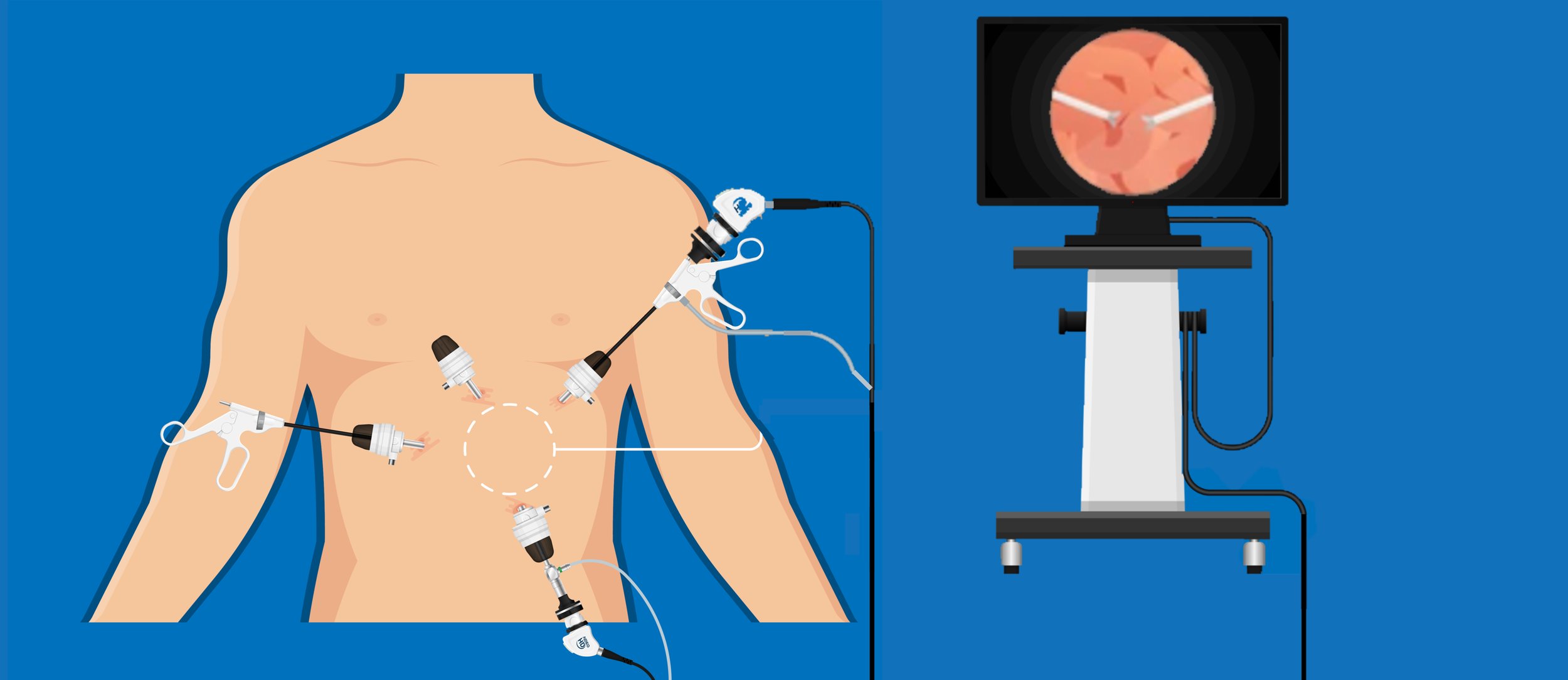
You will be given a general anesthetic, and will be asleep during the whole procedure. The surgery is performed through a series on small incisions. The first small cut is near your belly button where carbon dioxide gas is inserted into your peritoneal cavity- the space where most of your abdominal and pelvic organs lie. The gas expands the cavity assisting the surgeon to visualize your organs clearly. The surgeon then inserts the laparoscope (a thin fibro optic tube with camera and light attached) through other small cuts in your abdomen to explore the area and look at the organs. The image results are viewed on a screen in the operating room. When the surgeon is finished the laparoscope and gas is removed. The small cuts are closed with dressings; they are small and will heal quickly. You will then be woken up from the anesthetic and taken to the recovery room where a nurse will continue to monitor until you are ready to go up to the ward.
What to expect after your operation?
When you arrive back on the ward the nurse will continue to monitor you closely for the next four hours. The nurse will also be monitoring your pain levels. You can expect some soreness and pain around the small wound sites. This is normal and your nurse will encourage you to take some pain relief medication.
You may feel sleepy drowsy until the anaesthetic has worn off. You will have an oxygen mask in place until you become alert and awake. You will initially have fluids running through an intravenous cannula usually in hand of arm. This will be removed once you have tolerated diet and fluids. It is common for some individuals to feel nauseous and vomit after having anaesthetic. Your nurse will give you anti nausea medication to reduce the risk of this occurring.
Most patients are eating and drinking, gently ambulating, and have well controlled pain relief 24 hours post surgery and can expect to be discharged home.
At Discharge
You may be given some discharge medication (usually pain relief tablets), an outpatients appointment and medical certificate if requested. A discharge letter will be faxed to your local doctor.
Your doctor will inspect your wound sites at the follow up appointment and answer questions regarding your procedure. You should observe the sites for excessive bleeding, and signs and symptoms of infection such as pain, heat, redness, swelling or pus. If you have any concerns call you local doctor or treating hospital for further advice.
This information is intended as a guideline only. If you have any further questions or concerns, please ask your doctor.