Gastrectomy
What is a Gastrectomy?
The removal, or partial removal, of the stomach is known as a gastrectomy. The stomach is a hollow muscular organ that breaks down the food you eat into a semi-solid form so nutrients can then be absorbed into the blood stream as it passes into the small bowel. A person can adjust to living without a stomach. The digestive process continues in the remaining portion of the stomach. If all the stomach is removed the process begins in the small intestine. Dietary changes may be necessary and the body eventually adapts.
Who will need a gastrectomy?
A gastrectomy is used to treat stomach problems that aren’t helped by other treatments. Your doctor may recommend a gastrectomy to treat:
benign, or non-cancerous tumours
bleeding
inflammation
perforations in the stomach wall
polyps, or growths inside your stomach
stomach cancer
severe peptic or duodenal ulcers
What happens during the operation?
The operation starts once the anaesthetist has put you under a general anaesthetic. A gastrectomy can be performed either laparoscopically (key-hole) or with an open technique, dependent on your specific medical requirements. Your surgeon will discuss this with you before your procedure. With a laparoscopic technique, four or five small cuts are made in the abdomen to allow the surgeon to insert a laparoscope, and surgical tools. A laparoscope is a narrow telescopic video camera passed through a very small cut in the abdomen. It allows the surgeon to view magnified images of internal organs on a video monitor. With an open technique, a cut or incision is made from the breastbone to the umbilicus (belly button).
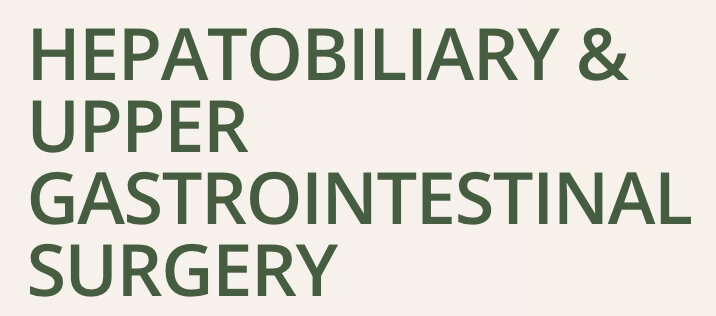
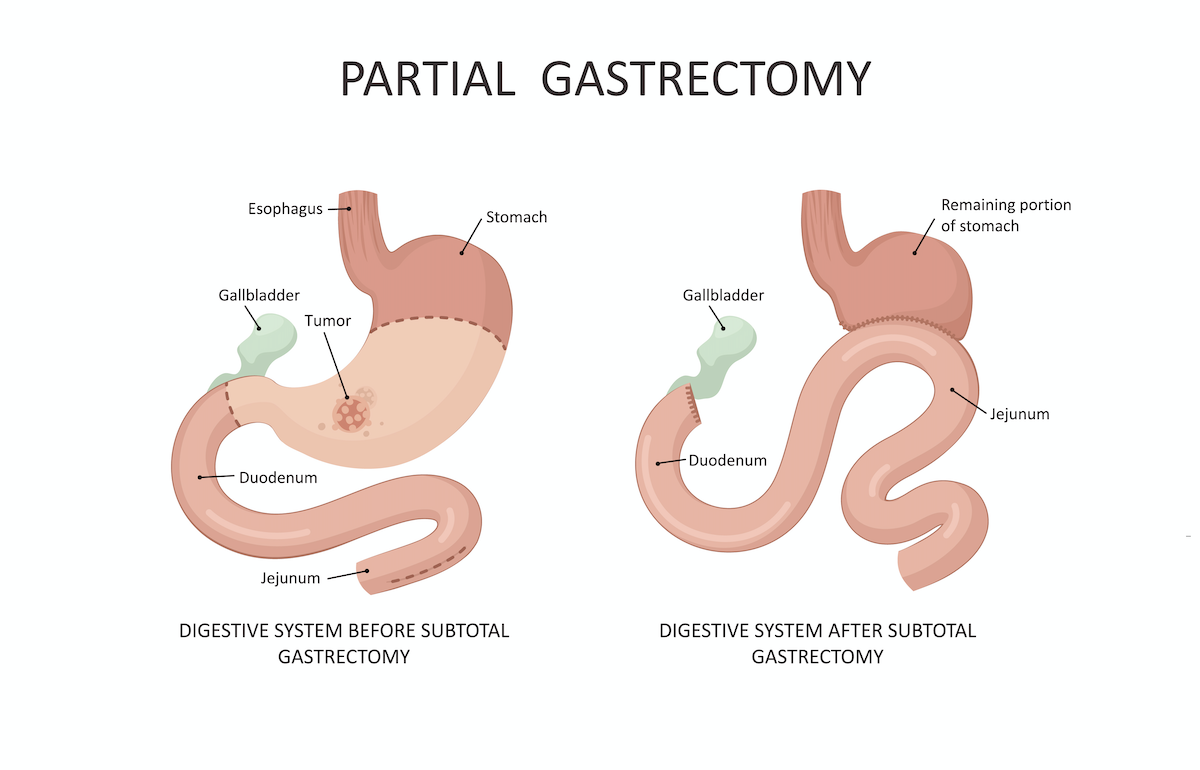
If the whole stomach is to be removed this is called a total gastrectomy. The oesophagus is then joined to the small intestine. A partial gastrectomy involves the removal of only some of the stomach. This is then rejoined making the area of the stomach much smaller. Close to the stomach are small lymph nodes (which can be found throughout the body), which filter out bacteria and other harmful agents. If you are having a gastrectomy as part of your treatment for cancer, the lymph nodes close to the stomach as well as the surrounding fatty tissue are removed to help prevent the spread of cancer to other areas of the body.
What to expect after your operation
Activity
You will be expected to sit in a chair for a short period of time the first day after your surgery. Activity will be increased, as you are able with the support of nursing staff and physiotherapists. You will need to wear an oxygen mask for a short time after your surgery to support your breathing. The amount of oxygen you will require will slowly be decreased as you recover. You will be constantly reminded to do your deep breathing and coughing exercises to help prevent chest infections. You will also be encouraged to exercise your legs, as lying still increases the risk of blood clots forming in your legs. Your nurse can assist you with balancing the need for activity with the need for rest.
Diet
Immediately after the surgery you be allowed sips of water, and you will slowly progress to greater volumes of clear and free fluids over the next few days. To help the body get all the nutrients it needs, you will usually have a feeding tube (known as a jejunostomy) inserted during surgery. A jejunostomy tube is a tube that is inserted into a part of the small intestine called the jejunum. These types of tubes are used when the stomach is unable to be used for feeding.
You may need to continue using your feeding tube for a few weeks to months after your surgery so you get all the nutrients you need when you are not eating and drinking well after your gastrectomy. Your dietitian will provide advice on this.
Your dietary requirements change for life after this operation. After your operation you will be seen by a dietitian who will advise you in this area. You may not go home until you have been seen by the dietitian. Essentially, you must now eat small frequent meals rather than 3 large meals per day.
Pain Management
Pain relief can be given in a number of ways including intravenously (via the drip) or by epidural anaesthesia, which involves placing a small tube into a part of your spinal cord called the epidural space prior to surgery and continuously infusing a drug to these pain nerves in the spinal cord. The anaesthetist will decide which of these forms of pain relief is most appropriate for you. An epidural should keep you comfortable for four to five days or until it is removed. You will also be given regular Panadol and anti-inflammatories (if appropriate). These medications will be given to you as suppositories until you are allowed to eat and drink. A urinary catheter is inserted during your surgery to monitor your urine output. This will be removed along with your epidural.
It is important that you are able to practice deep breathing and cough following your surgery to help prevent chest infections. Every endeavour will be made to ensure that you are comfortable enough to do this.
Wound Care
You will have several small cuts on your abdomen. Initially you will have a dressing covering these, but they will be removed 2 days after your surgery. You may then get your wound wet in the shower. There will be staples in situ; these will be removed prior to your discharge from hospital. A drain tube is inserted into the abdomen through the skin for drainage of blood and other fluids from around the operation site and is removed once drainage has reduced.
At Discharge
You will have a review appointment scheduled for you in the surgical outpatients clinic several weeks after your operation to review pathology results, monitor progress and recovery and discuss further treatment, if required. You may resume your normal activities, as you feel able. Do not return to work, driving and sporting activities until you have returned for your follow up appointment. Avoid heavy lifting and straining and ensure adequate support of your abdomen.
This information is intended as a guideline only. If you have any further questions or concerns, please ask your doctor.