Cancer Care Pathway for Gastric Cancer
FACTS
2000 Australians are diagnosed with gastric cancer annually
Gastric cancer is 2 times more common in men
Makes up 1.5% of all new cancers cases diagnosed in 2020
SYMPTOMS
Indigestion
Frequent burping
Heartburn/Reflux
Feeling “full” after a small meal
Ongoing nausea and/or vomiting
Loss of appetite
Unintentional weight loss
Abdominal swelling/bloating
Blood when vomiting
Fatigue
What is Gastric Cancer?
Gastric cancer refers to cancer of the stomach. There are four layers that make up the stomach these include:
Mucosa: this is where the fluid is produced that help to commence the breakdown of food, also known as “digestive enzymes”
Submucosa: this layer provides the stomach with blood and nutrients
Muscle layer (Muscularis): as a muscle, this layer contracts and assists to breakdown your food and push it in to the digestive system
Outer layer (Subserosa): smooth muscle layer around the stomach.
The most common type of gastric cancer starts in the mucosal layer and is termed “adenocarcinoma”. This makes up 90-95% of gastric cancers.
To make a diagnosis of gastric cancer, the first thing you will be asked is about your past medical history, your family history of cancer and your current symptoms. The symptoms of gastric cancer are listed to the left.
To confirm your diagnosis, your GP, gastroenterologist or surgeon will organise a series of tests.
Diagnosis: What to Expect
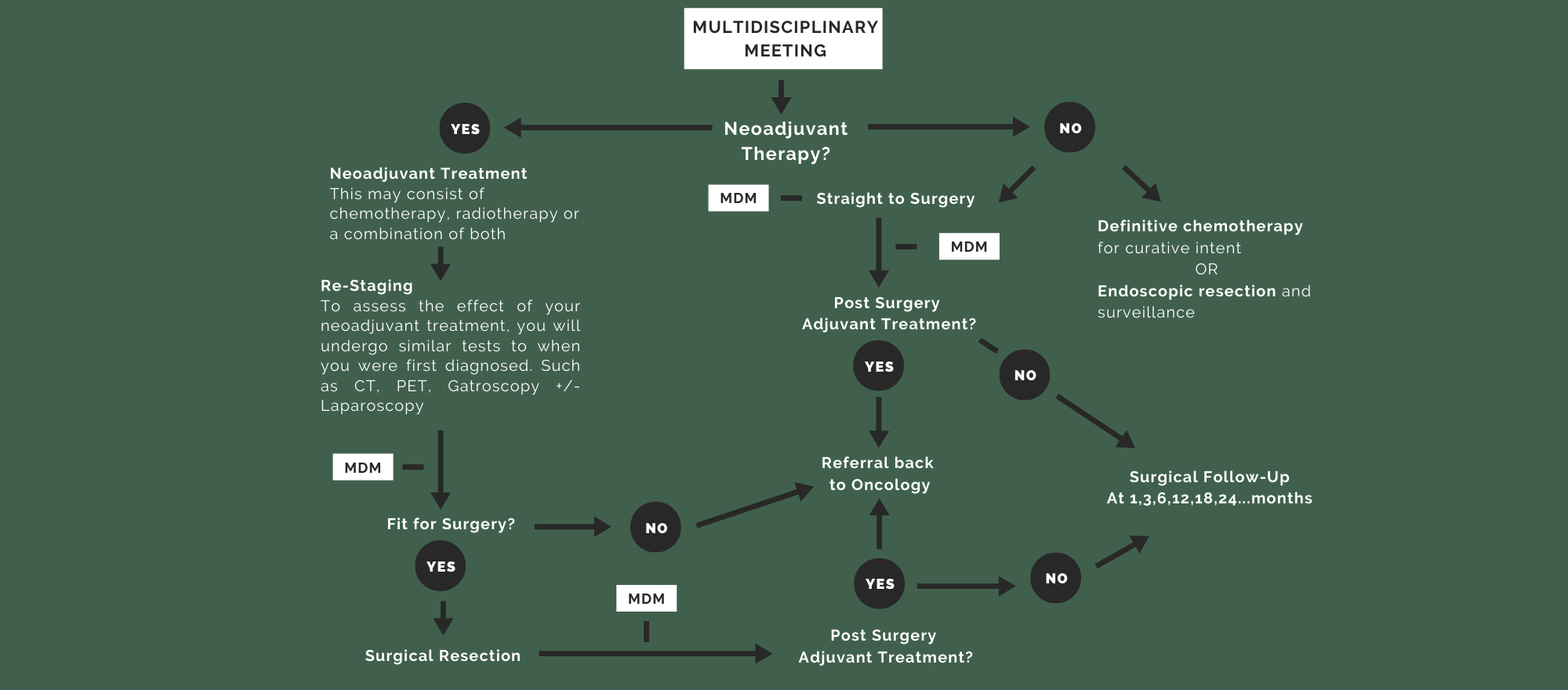
Multidisciplinary Meeting
After your investigations have been completed, your case will be discussed at a multidisciplinary meeting (MDM). This meeting is made up of surgeons, oncologists, radiologists, pathologists and the allied health team to collaboratively discuss your diagnosis and determine the best individualised treatment pathway for your disease. Your cancer will be staged by what is referred to as the “TNM” Staging System. Once this has been determined, you will meet with your surgeon again. This will take you through to the treatment phase of your journey.
Treatment Team
-

Surgeon
At this appointment, you will meet with the surgeon, fellow or registrar to discuss your diagnosis and treatment options. If this includes surgery, the surgeon will talk you through the operation, risks and benefits so that you can make informed decisions.
-

Cancer Nurse Coordinator
Your meeting with the cancer nurse may coincide with any of the above appointments depending on your treatment. Here, you will be provided with contact details for a central contact at the hospital, educational resources and you will have the opportunity to ask any questions you have about your care.
-
Medical/Radiation Oncologist
If your treatment involves pre-operative chemotherapy (known as neoadjuvant treatment), you will meet the medical oncologist. At this point, you may also meet the radiation oncologist. The oncologists work collaboratively with the surgeons to ensure you are receiving the best care possible.
-
Anaesthetist
Will assess your fitness for surgery and talk you through the medications and pain relief administered during the surgery.
-
Dietitian
Some of you will be referred to a dietitian at the time of diagnosis. This will give you an opportunity to optimise your nutrition prior to treatment and allow ongoing support both in and out of the hospital.
-

Physiotherapist
Will guide you in enhancing your physical fitness for pre-habilitation before surgery and in mobilising and keeping active after surgery.
-

Psych-Oncologist
Will review mental health issues related with your cancer diagnosis.
Please Note: If you are having surgery, you will also meet a number of people involved in your “Pre-Surgery” planning and assessment. Your Cancer Nurse Coordinator will take you through this in more detail during your appointment.

Resources
A Common Path: Oesophagastric Cancer - Victorian Integrated Cancer Services
Oesophagogastric Cancer - Your Guide to Best Cancer Care, Cancer Council
Understanding Stomach and Oesophageal Cancers - Cancer Council Victoria