Cancer Care Pathway for Oesophageal Cancer
FACTS
Oesophageal cancer is uncommon
Makes up 1.4% of cancer cases in men and 0.8% in women in Australia
1587 were diagnosed with Oesophageal cancer in 2020
SYMPTOMS
Unexplained weight loss
Difficulty swallowing
Food or fluids getting stuck in your throat
Episodes of choking
Vomiting blood
New or worse heartburn and reflux
What is Oesophageal Cancer?
Oesophageal cancer refers to a malignant tumour found in the oesophagus, more commonly known as your food pipe.
The oesophagus is essential in your digestion and nutrition as it connects the mouth to the stomach. The oesophagus is lined with muscle which allows you to push your food down to your stomach. An oesophageal tumour may be found at various points within the oeosphagus, but it is most commonly found at the lower end– where the stomach and oesophagus meet. This is called the Gastro-Oesophageal Junction.
There are two types of cancers found in the oesophagus, you may hear your surgeon refer to either of the following:
Adenocarcinoma
Squamous cell carcinoma
The type of cancer will determine the treatment decision. The oesophagus has a number of layers, and the above cancer types are the medical terms used when discussing your cancer. They refer to the specific layers of the oesophagus and the cells affected by your cancer. If you’d like to learn more– ask your Surgeon or Cancer Nurse Coordinator to explain this to you in more detail.
In order to diagnose your cancer, read on to learn about the various tests and procedures that you may undertake prior to diagnosis.
Diagnosis: What to Expect
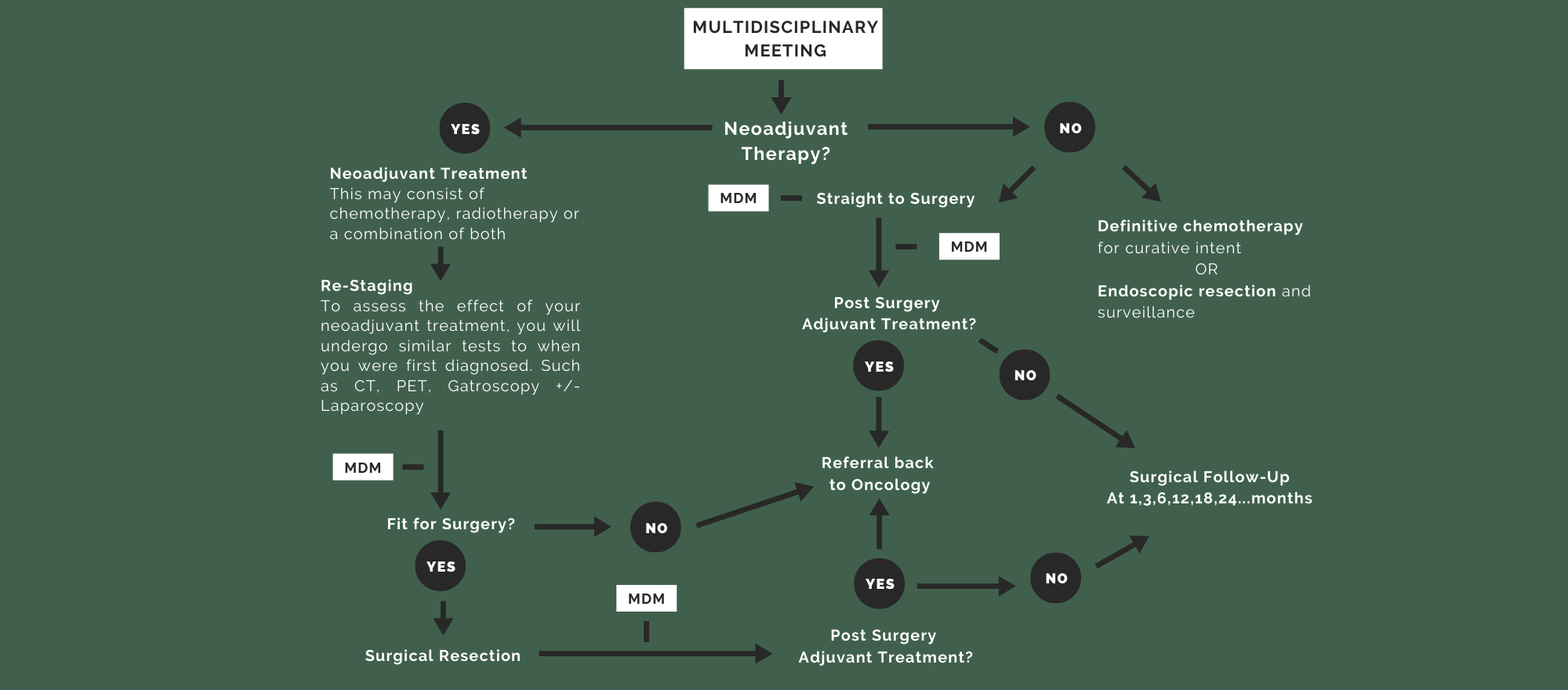
Multidisciplinary Meeting
After your investigations have been completed, your case will be discussed at a multidisciplinary meeting (MDM). This meeting is made up of surgeons, oncologists, radiologists, pathologists and the allied health team to collaboratively discuss your diagnosis and determine the best individualised treatment pathway for your disease. Your cancer will be staged by what is referred to as the “TNM” Staging System. Once this has been determined, you will meet with your surgeon again. This will take you through to the treatment phase of your journey.
Treatment Team
-

Surgeon
At this appointment, you will meet with the surgeon, fellow or registrar to discuss your diagnosis and treatment options. If this includes surgery, the surgeon will talk you through the operation, risks and benefits so that you can make informed decisions.
-

Cancer Nurse Coordinator
Your meeting with the cancer nurse may coincide with any of the above appointments depending on your treatment. Here, you will be provided with contact details for a central contact at the hospital, educational resources and you will have the opportunity to ask any questions you have about your care.
-

Medical/Radiation Oncologist
If your treatment involves pre-operative chemotherapy (known as neoadjuvant treatment), you will meet the medical oncologist. At this point, you may also meet the radiation oncologist. The oncologists work collaboratively with the surgeons to ensure you are receiving the best care possible.
-

Anaesthetist
Will assess your fitness for surgery and talk you through the medications and pain relief administered during the surgery.
-

Dietitian
Some of you will be referred to a dietitian at the time of diagnosis. This will give you an opportunity to optimise your nutrition prior to treatment and allow ongoing support both in and out of the hospital.
-

Physiotherapist
Will guide you in enhancing your physical fitness for pre-habilitation before surgery and in mobilising and keeping active after surgery
-

Psych-Oncologist
Will review mental health issues related with your cancer diagnosis.
Please Note: If you are having surgery, you will also meet a number of people involved in your “Pre-Surgery” planning and assessment. Your Cancer Nurse Coordinator will take you through this in more detail during your appointment.

Resources
A Common Path: Oesophagastric Cancer - Victorian Integrated Cancer Services
Oesophagogastric Cancer - Your Guide to Best Cancer Care, Cancer Council
Understanding Stomach and Oesophageal Cancers - Cancer Council Victoria